Reticulocytes: A complete guide to understanding your blood test
Blood test results are often filled with technical terms and values that can seem mysterious. Understanding a key marker like reticulocytes is essential. It provides valuable insight into your overall health. This knowledge can help you better understand your lab results. This article will explain reticulocytes and give you the keys to interpret this crucial value.
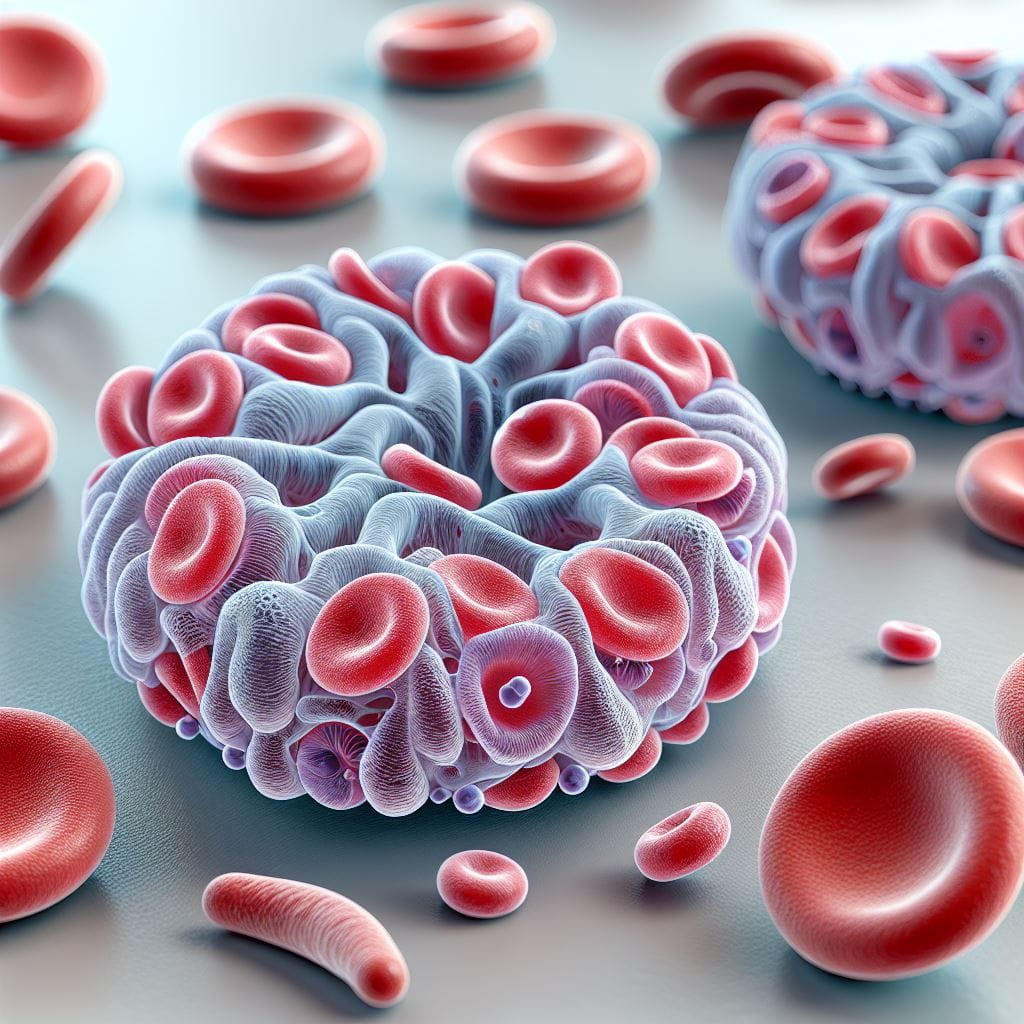
What are reticulocytes? A simple definition
Reticulocytes are young, immature red blood cells. Think of your bone marrow as a factory that builds vehicles to transport oxygen. In this analogy, reticulocytes are cars just leaving the assembly line. They are released into your bloodstream while they still contain remnants of genetic material, specifically RNA.
Typically, these young cells circulate in the blood for about 24 to 48 hours. During this period, they finish maturing into erythrocytes, or fully developed red blood cells. This process occurs naturally within your circulatory system. Therefore, reticulocytes are reliable indicators of your bone marrow’s production activity. For instance, if your body detects low tissue oxygenation, it boosts reticulocyte production. This happens with anemia or during a stay at high altitude. This process is regulated by erythropoietin (EPO), a hormone mainly produced by your kidneys.
A doctor orders a reticulocyte count to evaluate the bone marrow’s ability to produce new red blood cells. The test is especially useful for identifying the cause of anemia. It also helps monitor the effectiveness of a treatment.
Why understanding your reticulocytes matters
Reticulocytes are not an isolated indicator. They are part of a complex set of blood parameters. Together, these markers paint a detailed picture of your hematological health. They interact with other key markers like hemoglobin and hematocrit. This creates a coherent clinical profile.
The importance of this marker is well-established. Overlooking an abnormal reticulocyte count can have significant consequences. For example, a chronically low count may hide a serious condition where the bone marrow doesn’t produce enough blood cells. Careful monitoring can lead to earlier detection of such issues.
Furthermore, many treatment decisions rely on this analysis. For a patient with anemia, a high reticulocyte count suggests the bone marrow is healthy, but red blood cells are being destroyed too quickly. This is characteristic of hemolytic anemia. In contrast, a low count would suggest a production problem in the marrow. These two scenarios require completely different therapeutic approaches. This highlights the crucial importance of the reticulocyte count.
How to read and interpret your lab results
When you receive your blood work, you will see reticulocyte results listed in several ways.
Common measurements on your report
- The absolute number of reticulocytes. Normal reference values are typically 25,000 to 85,000 cells per microliter (μL).
- The percentage of reticulocytes. This is their share among all red blood cells. Normal reference values are 0.5% to 2.0%.
- The Reticulocyte Production Index (RPI). This calculation adjusts the percentage based on the severity of anemia.
On your lab report, pay attention to the color code. Red usually flags values outside the normal range. Black or green indicates normal values. Some labs also use arrows (↑ or ↓) to show if a value is above or below the reference range.
Understanding reference values
Labs establish their own reference values for reticulocytes. They do this by studying large populations of healthy individuals. These values may vary slightly between labs due to different analysis methods and equipment. Additionally, reference values can differ based on age, sex, and even altitude.
A tip for a quick assessment
Here is a practical way to quickly interpret your results. Always compare your reticulocyte count with your hemoglobin level. If you have anemia (low hemoglobin) and a high reticulocyte count, it suggests your bone marrow is responding well. However, if both hemoglobin and reticulocytes are low, this may point to a problem at the production level in the marrow.
Conditions related to high reticulocyte counts
An increased number of reticulocytes usually signals that the bone marrow is overproducing red blood cells. This is generally a response to blood loss or cell destruction.
Hemolytic anemia
This condition involves the premature destruction of red blood cells. It triggers a strong response from the bone marrow. The marrow speeds up the production of new red blood cells, which increases the reticulocyte count. Specific symptoms can include severe fatigue, yellowing of the skin (jaundice), and dark urine.
Acute hemorrhage
In the event of significant blood loss, the body responds by boosting the production of new blood cells. This response includes an increase in reticulocytes to replace the lost cells. Symptoms often include pallor, a rapid heart rate, and low blood pressure.
Response to anemia treatment
Effective treatment for anemia often causes an increase in reticulocytes. This happens about 3 to 5 days after starting therapy with iron, vitamin B12, or folic acid. This rise is a positive sign. It indicates that bone marrow activity is restarting properly.
What a low reticulocyte count means
A low reticulocyte count suggests the bone marrow is not producing enough red blood cells to meet the body’s needs.
Aplastic anemia
This is a serious condition resulting from bone marrow failure. The marrow can no longer produce enough blood cells, including the precursors to reticulocytes. Symptoms include extreme pallor, debilitating fatigue, frequent infections, and spontaneous bleeding.
Nutritional deficiency anemia
A deficiency in essential elements like iron, vitamin B12, or folic acid harms red blood cell production. As a result, the reticulocyte count will be low. Associated symptoms include chronic fatigue and brittle hair and nails.
Chronic kidney disease
Poorly functioning kidneys produce too little erythropoietin (EPO). EPO is the hormone that stimulates red blood cell production. Without enough EPO, the reticulocyte count falls. Symptoms can include shortness of breath, edema, and high blood pressure.
Practical tips for follow-up and action
Always discuss your results with a healthcare provider. They can provide context based on your personal health profile.
Suggested follow-up schedule
- Mild abnormality: With your doctor’s agreement, a follow-up in 3 months may be appropriate.
- Moderate abnormality: A re-check in 4-6 weeks is often recommended.
- Severe abnormality: Closer monitoring may be needed, sometimes weekly until the values stabilize.
When to see a specialist
It is crucial to know when a medical consultation is needed. Consult a doctor promptly if:
- Your reticulocyte count is extremely low or very high.
- You have accompanying symptoms like severe fatigue, shortness of breath, or dizziness.
- Several blood parameters are abnormal at once.
- You notice a rapid decline in your values between tests.
Simple monitoring may be enough if the abnormality is mild and isolated, your values are stable, and you have no concerning symptoms.
Frequently asked questions about reticulocytes
Does the reticulocyte count vary during the day?
The reticulocyte count does not show significant daily variation. However, intense exercise or a recent change in altitude can influence results. For reliable results, it is best to have your blood drawn in the morning.
How does age affect the normal reticulocyte range?
Newborns naturally have higher reticulocyte counts (2% to 6%). These values decrease to adult levels by about 2-3 months of age. In older adults, the lower limit may dip slightly, reflecting a reduced bone marrow response.
Can you have a normal reticulocyte count with severe anemia?
Yes, this situation is called an “inappropriate reticulocyte response.” The count is technically normal but is insufficient for the severity of the anemia. This is why clinicians often calculate the Reticulocyte Production Index (RPI) to get a clearer picture.
Do medications interact with the reticulocyte count?
Yes, several medications can affect your count. Chemotherapy and immunosuppressants generally decrease production. Conversely, EPO treatments significantly increase it. Always inform your doctor about all medications you are taking.
How do you differentiate a high count from anemia versus altitude?
Acclimatization to altitude causes a moderate, gradual increase in reticulocytes. This is followed by a rise in hemoglobin. In contrast, the increase in hemolytic anemia is often more pronounced. It is also accompanied by low or falling hemoglobin and other specific markers.
Conclusion: Your key to blood health
Reticulocytes are a direct window into your bone marrow’s activity. Understanding this marker helps to detect blood disorders, differentiate types of anemia, and evaluate treatments. In an age of personalized medicine, understanding your biological data is essential. Now is the time to take an active role in your health. By staying informed and talking with your doctor, you can turn your results into a concrete action plan for your well-being.
Further Resources
To deepen your understanding about reticulocytes and blood tests, here is a reliable resource:
Decode Other Markers
You may also like

Insulin blood test: Understanding your levels and what they mean

Glycated hemoglobin (HbA1c): Your complete guide

Fasting blood glucose: Your complete guide to interpretation
