Reticulocytes: The Complete Guide to Understanding Your Blood Test
Have you ever felt a twinge of anxiety while looking over your blood test results? These documents are often filled with technical jargon and values that can seem mysterious. Faced with these figures—sometimes highlighted in red—a simple medical checkup can turn into a source of stress. Among these data, reticulocytes frequently raise questions. Yet, understanding this blood marker is essential. It provides valuable insight into your overall health and can significantly reduce your apprehension about lab results. This article aims to familiarize you with reticulocytes and give you the keys to interpreting this crucial value.
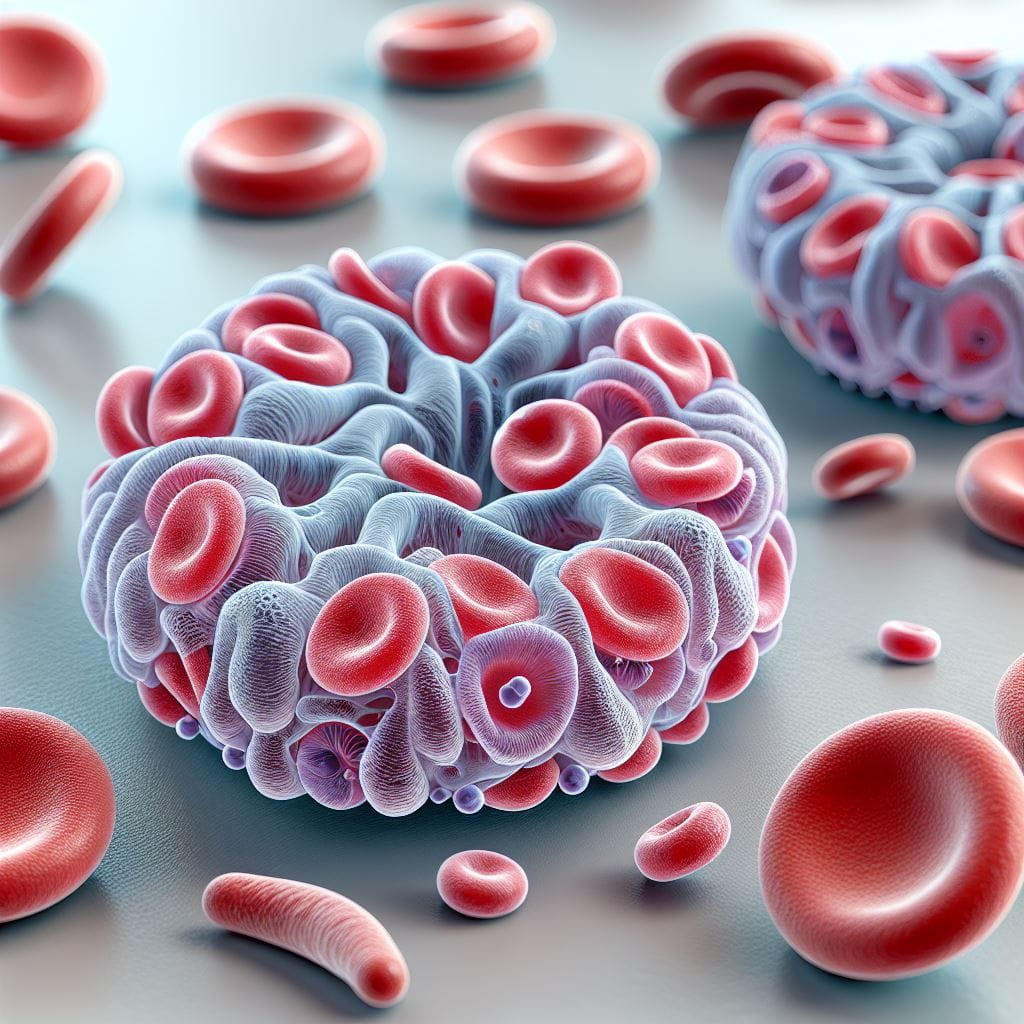
What Are Reticulocytes? A Simple Definition
Reticulocytes, sometimes called “retics” in medical slang, are young red blood cells. They have not yet reached full maturity. Picture your bone marrow as a factory making vehicles that transport oxygen. In this analogy, reticulocytes are like cars leaving the assembly line before the paint is fully dry. Indeed, these cells are released into your bloodstream while they still contain remnants of genetic material—specifically, RNA.
Typically, these young red blood cells circulate in the blood for about 24 to 48 hours. During this time, they complete their maturation and become erythrocytes, or fully mature red blood cells. This developmental process occurs naturally within your circulatory system. Thus, reticulocytes play a fundamental role: they serve as reliable indicators of your bone marrow’s red blood cell production activity. For example, if your body detects low oxygenation of the tissues—such as in anemia or during a stay at high altitude—it responds by increasing the production of reticulocytes to boost oxygen-carrying capacity. This ingenious process is regulated by erythropoietin (EPO), a hormone mainly produced by your kidneys, which stimulates the bone marrow.
A doctor usually orders a reticulocyte count. This test evaluates your bone marrow’s ability to produce new red blood cells. It is especially useful for identifying the cause of anemia or for monitoring the effectiveness of a treatment aimed at correcting abnormalities in red blood cell production.
Why Understanding Your Reticulocytes Matters
Reticulocytes are not an isolated indicator. They are part of a complex set of blood parameters that together paint a detailed picture of your hematological health. Consider your blood system as a symphony: every instrument plays its part. Reticulocytes offer their unique note to this harmony. They interact with other key markers—notably hemoglobin, hematocrit, and various red cell indices—that make up a coherent clinical profile.
The scientific story of reticulocytes dates back to the early 20th century, when researchers developed specific staining techniques to distinguish these young cells from mature red blood cells. Since then, our understanding of their clinical significance has constantly evolved. Recent studies have even shown that tracking reticulocytes provides an early diagnostic tool for various diseases—alerting physicians long before obvious clinical symptoms appear.
Overlooking an abnormal reticulocyte count can lead to significant long-term consequences. For example, a chronically low count without proper medical follow-up may hide bone marrow aplasia—a potentially serious condition where the marrow doesn’t produce enough blood cells. Recent data show that about 12% of unexplained anemias are linked to reticulocyte production abnormalities. Careful monitoring could have led to earlier detection.
Treatment decisions often rely on reticulocyte analysis. Consider a real-life example: a doctor treating a patient with anemia. If the test shows an elevated reticulocyte count, this indicates healthy bone marrow activity but also that red blood cells are being destroyed too quickly—characteristic of hemolytic anemia. Conversely, a low count would suggest a problem with marrow production. These two scenarios require radically different therapeutic approaches. According to medical statistics, over 30% of treatment decisions for hematological disorders are based directly on the interpretation of the reticulocyte count and its changes—highlighting their crucial importance.
How to Read and Interpret Your Lab Results?
When you receive your blood work, reticulocyte results may be listed in several ways. Typically, you’ll see the following information:
- The absolute number of reticulocytes (normal reference values: 25,000 to 85,000 cells/μL).
- The percentage of reticulocytes among all red blood cells (normal reference values: 0.5% to 2.0%).
- The Reticulocyte Production Index (RPI), which adjusts the percentage based on the severity of anemia.
On your lab report, pay attention to the color code. Usually, red flags values outside the normal range, while black or green indicate normal values. Some labs also use symbols, such as arrows (↑ or ↓), to indicate whether a value is above or below the reference range.
Understanding Reference Values
Labs set their own reference values for reticulocytes by studying large populations of healthy individuals. These values may vary slightly between labs, depending on analysis methods and equipment. Additionally, reference values may differ based on age, sex, and even the altitude at which the patient lives.
Tip for a Quick First Assessment
Here’s a practical shortcut for quickly interpreting your results: always compare your reticulocyte count with your hemoglobin level. If you have anemia (low hemoglobin) and elevated reticulocytes, this suggests your bone marrow is responding well. However, if both hemoglobin and reticulocytes are low, this may indicate a problem at the marrow production level.
Conditions Related to Reticulocyte Counts
Abnormal reticulocyte levels can reveal various conditions. We can classify them by frequency and severity.
High Reticulocyte Count: What Are the Causes?
An increased number of reticulocytes usually signals that the bone marrow is overproducing red blood cells, generally in response to loss or destruction.
Hemolytic Anemia
- Frequency: High.
- Severity: Moderate to severe.
- Mechanisms: This condition involves premature destruction of red blood cells. It triggers a compensatory response from the bone marrow, which speeds up the production of new red blood cells—hence the increase in reticulocytes.
- Specific symptoms: Severe fatigue, yellowing of skin and eyes (jaundice), dark urine.
- Additional tests: Direct Coombs test, serum haptoglobin measurement, search for schistocytes on a blood smear.
Acute Hemorrhage
- Frequency: Moderate.
- Severity: Variable depending on the cause.
- Mechanisms: In the event of significant blood loss, the body responds by boosting production of new blood cells, including reticulocytes.
- Symptoms: Pallor, rapid heart rate (tachycardia), low blood pressure (hypotension).
- Further tests: Search for hidden bleeding, digestive endoscopy, CT scan depending on clinical suspicion.
Response to Anemia Treatment
- Frequency: High.
- Severity: Low (a positive sign).
- Mechanisms: Effective treatment of anemia (for example, iron, vitamin B12, or folic acid supplementation) causes an increase in reticulocytes about 3 to 5 days after starting therapy. This indicates bone marrow activity is restarting.
- Example: Mrs. D., 45, had iron-deficiency anemia with an initially low reticulocyte count. After 10 days of iron supplementation, her count rose from 0.2% to 3.5%, signaling an appropriate bone marrow response.
Low Reticulocyte Count: What Does It Mean?
A low reticulocyte count suggests the bone marrow isn’t producing enough red blood cells to meet the body’s needs.
Aplastic Anemia
- Frequency: Low.
- Severity: High.
- Mechanisms: This serious condition results from bone marrow failure, which can no longer produce enough blood cells, including reticulocyte precursors.
- Symptoms: Extreme pallor, debilitating fatigue, frequent infections, spontaneous bleeding.
- Further investigation: Bone marrow biopsy, marrow karyotype analysis.
Nutritional Deficiency Anemia
- Frequency: High.
- Severity: Moderate.
- Mechanisms: Deficiency in essential elements such as iron, vitamin B12, or folic acid prevents normal production of red blood cells—and thus reticulocytes.
- Associated symptoms: Chronic fatigue, brittle hair and nails, sometimes neurological issues (especially with B12 deficiency).
- Additional tests: Complete iron profile, serum vitamin B12 and folate assays.
Chronic Renal Failure
- Frequency: Moderate.
- Severity: High.
- Mechanisms: Poorly functioning kidneys produce too little erythropoietin (EPO), the hormone that stimulates red blood cell—and therefore reticulocyte—production.
- Symptoms: Shortness of breath during exertion, edema, high blood pressure.
- Workup: Complete kidney function panel (including creatinine clearance), serum EPO measurement.
A clinical case clearly illustrates this: Mr. R., 67, had moderate anemia (hemoglobin 10.2 g/dL) with a particularly low reticulocyte count (0.1%). Investigations revealed myelodysplastic syndrome—a bone marrow disorder that can progress to leukemia. This case underscores the diagnostic importance of the reticulocyte count for spotting potentially serious conditions.
Practical Tips for Action and Follow-Up
Suggested Follow-Up Schedule Based on Abnormalities
- Mild abnormality (slightly abnormal reticulocyte count, isolated): Consider a follow-up in 3 months with your doctor’s agreement.
- Moderate abnormality: A re-check in 4-6 weeks is often recommended.
- Severe abnormality: Closer monitoring may be needed, sometimes weekly until stabilization.
Specific Dietary Advice
If your reticulocyte count is low and nutritional deficiency is suspected, enrich your diet with:
- Iron: Lean red meat, lentils, spinach, tofu.
- Vitamin B12: Dairy products, eggs, fish.
- Folic acid (Vitamin B9): Green leafy vegetables (spinach, broccoli), citrus fruits, legumes.
If you have elevated reticulocytes due to hemolysis (excessive destruction of red blood cells), focus on:
- Antioxidants: Berries (blueberries, raspberries), nuts, oily fish rich in omega-3s.
- Adequate hydration: Drink at least 1.5 to 2 liters of water per day.
- Alcohol reduction: Alcohol may worsen certain types of hemolytic anemia.
Lifestyle Changes to Optimize Your Red Blood Cell Production
To encourage healthy red blood cell production and potentially improve your reticulocyte count:
- Engage in moderate, regular physical activity.
- Reduce chronic stress, which can affect bone marrow function.
- Ensure quality sleep (about 7-8 hours per night).
- Avoid exposure to toxic substances (tobacco, heavy pollution).
When to See a Specialist, and When Is Simple Monitoring Enough?
It’s crucial to know when a medical consultation is needed.
Consult a Doctor or Specialist Promptly If:
- Your reticulocyte count is extremely low (e.g., <0.1% or below your lab’s thresholds) or very high (e.g., >5% or above thresholds).
- You have accompanying symptoms such as severe, unusual fatigue, pronounced shortness of breath, or frequent dizziness.
- Several blood parameters are abnormal at once.
- You notice a rapid decline in your values between tests.
Simple Monitoring May Be Enough If:
- The reticulocyte abnormality is mild and isolated (no other major blood parameter is affected).
- Your values remain stable in follow-up tests.
- You have no concerning symptoms.
- Your doctor has specifically told you that monitoring alone is sufficient in your situation.
Tips to Potentially Improve Your Values Naturally
While these tips don’t replace medical advice or treatments, certain habits can support good blood health:
- Get sun exposure (about 15-20 minutes daily, with skin protection) to boost vitamin D synthesis, which is involved in many bodily processes.
- Incorporate copper-rich foods (seafood, nuts, pulses), an important trace element.
- Limit tea and coffee during meals, as they can reduce iron absorption.
- Consume vitamin C (citrus, bell peppers, kiwis) together with iron-rich foods to improve absorption.
Frequently Asked Questions About Reticulocytes
Does the Reticulocyte Count Vary During the Day?
Unlike some other blood parameters—such as cortisol—the reticulocyte count doesn’t show significant circadian variation. However, factors like intense physical exercise, a recent change in altitude, or acute stress may temporarily influence your results. For more reliable and comparable results, it’s best to have your venous blood drawn in the morning—ideally fasting if other tests require it.
How Does Age Affect the Normal Reticulocyte Range?
Newborns naturally have higher reticulocyte counts (ranging from 2% to 6%) during the first weeks of life. These values gradually decrease to adult norms by the age of about 2-3 months. In elderly individuals (generally >75 years), the lower limit for reticulocytes tends to dip slightly. This may reflect a somewhat reduced bone marrow response with age.
Is It Possible to Have a Normal Reticulocyte Count Despite Severe Anemia?
Yes—this situation is called “inappropriate reticulocyte response.” In this case, the reticulocyte count, although apparently normal (absolute or percentage), is actually insufficient for the severity of anemia. That’s why clinicians often calculate the Reticulocyte Production Index (RPI). This index adjusts the reticulocyte count to the hematocrit (the volume of red blood cells in the blood). An RPI less than 2 in the presence of anemia generally suggests inadequate marrow response.
Are There Interactions Between Certain Medications and the Reticulocyte Count?
Several medication classes can affect your reticulocyte count. Chemotherapy agents and immunosuppressants, for example, generally decrease production by suppressing bone marrow activity. Conversely, erythropoietin (EPO) treatments significantly increase reticulocyte counts—typically 3-5 days after administration. Some antibiotics—like chloramphenicol (now rarely used for this reason)—can also reduce reticulocyte production. Always inform your doctor about all medications you are taking when interpreting your results.
Do Elite Athletes Have Different Reticulocyte Counts?
Intense and regular training—especially in endurance sports—can slightly raise the baseline reticulocyte count in athletes. This is due to the body’s physiological adaptation to prolonged effort and increased oxygen demand. That’s one reason the biological passport for athletes closely monitors this parameter. A sudden, significant rise could indicate EPO doping in specific contexts. Athletes also often show a quicker recovery of reticulocyte levels after blood donation or minor hemorrhage.
How to Differentiate Between an Increase in Reticulocytes Due to Anemia and That Due to Altitude?
Acclimatization to altitude causes a gradual increase in reticulocytes in response to lower oxygen pressure. This increase is typically moderate (rarely exceeding 3-4%) and is followed over days to weeks by a parallel rise in hemoglobin and hematocrit. In contrast, in hemolytic anemia (red blood cell destruction), the reticulocyte increase is often more pronounced (sometimes exceeding 10%) and accompanied by low or falling hemoglobin. The presence of other markers—such as high bilirubin or low haptoglobin—will shift the diagnosis toward hemolysis rather than simple adaptation to altitude.
Conclusion: Reticulocytes, a Key to Your Blood Health
Reticulocytes are much more than a simple number on your lab report. They are a direct window into your bone marrow’s activity and the renewal dynamics of your red blood cells. Understanding this marker allows you to:
- Detect certain blood disorders early.
- Help differentiate between types of anemia and their underlying causes.
- Evaluate the effectiveness of treatments for anemia.
- Optimize your medical follow-up by becoming an informed partner with your doctor.
In the age of personalized medicine, understanding your own biological data is an essential tool for empowerment. Interpretation platforms transform data once reserved for specialists into accessible, actionable information. Advances in this field are promising: new reticulocyte subtypes are being researched, which could allow even earlier and more accurate diagnosis of certain blood conditions. In addition, artificial intelligence algorithms are starting to incorporate reticulocyte variations into overall health prediction models.
Now is the time to take an active role in understanding your hematological health. Don’t wait for serious symptoms to appear before trying to decode your lab results. By staying informed and talking with your doctor, you can turn your results into a concrete action plan for your wellbeing.
Further Resources
To deepen your understanding about reticulocytes and blood tests, here is a reliable resource:
Decode Other Markers
You may also like

Protein S Test Results: Understanding Your Levels and Their Significance

Protein C Deficiency: A Complete Guide to Understanding Your Blood Test

ALT/SGPT : Decipher this key liver marker
